Vertebroplasty
What is vertebroplasty?
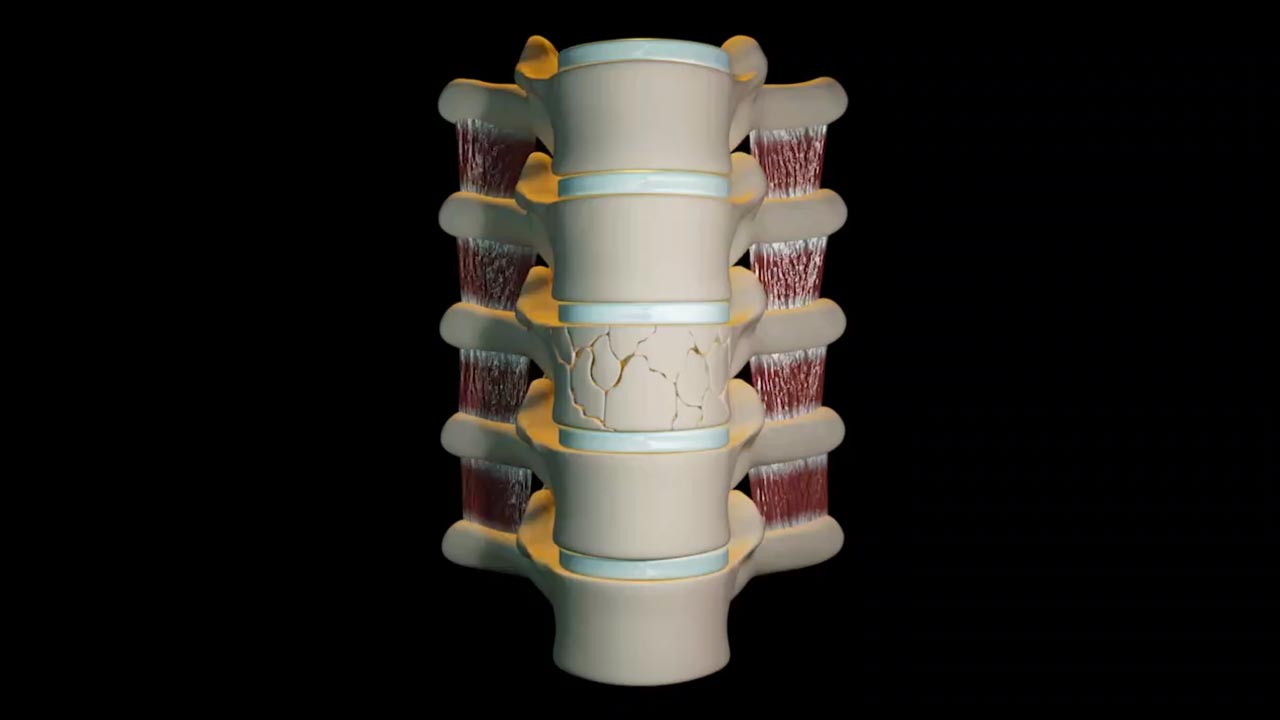
Vertebroplasty is a minimally invasive procedure used to stabilise and strengthen a collapsed spinal vertebra that has fractured and lost height due to osteoporosis, tumour infiltration or trauma.
Vertebroplasty is primarily aimed at relieving pain in order to promote a return to previous levels of activity and to also prevent further vertebral collapse. It is minimally invasive which means that patients suffer less disruption, face less risk and recover more quickly than with conventional open surgery. The procedure is most effective when the fracture has occurred relatively recently and particularly in patients who are very debilitated by pain and/or cannot tolerate adequate quantities of painkilling medication. In some circumstances, vertebroplasty can be effective even if the fracture is many months old but continues to cause significant discomfort and affects daily life.
The procedure is performed by introducing specially designed needles into the affected vertebra under the guidance of an X-ray camera. Bone cement is then injected through the needles into the fractured bone forming a cement cast which acts to stabilise the fracture and strengthen the affected bone. The principle is not dissimilar to using a plaster cast for a fracture of the leg.
Which patients are susceptible to vertebral fractures?
Osteoporotic compression fractures are most commonly encountered in post-menopausal women because hormonal changes reduce the quality of bone rendering them more prone to fracture. More than a quarter of women over age 65 will develop a vertebral fracture due to osteoporosis. Younger patients can also be affected by osteoporosis due to the long term use of steroid based medications.
Older people suffering from compression fractures tend to become less mobile and this decreased mobility further accelerates bone loss and also has a significant impact on cardiovascular fitness.
What tests and patient preparation are necessary before the procedure?
Prior to the procedure, all patients will have an MRI scan to confirm which vertebral bone(s) is/are fractured and to age the fractures. It is important to correlate the MRI findings with a thorough clinical examination ensuring that symptoms are attributable to a fracture of the spine and not an alternative cause. If you are unable to have an MRI, a CT of the spine can be used instead.
Medications that thin the blood (antiplatelet/anticoagulant) have to be stopped at least 5 days before the procedure. It may be necessary to commence another form of temporary blood thinner for a few days if deemed clinically necessary. This will be confirmed by your doctor prior to the procedure.
How is the procedure performed?
The procedure is performed in the Interventional Radiology Suite by a specially trained doctor called an interventional radiologist. The patient lies face down on an x-ray table and is given medications to reduce pain and discomfort and to make them sleepy. A dedicated nursing team will monitor and care for the patient throughout the procedure.
Following the injection of local anaesthetic into the skin and around the spine, hollow needles are passed into the fractured vertebral body under continuous X-ray guidance. Once these needles are in place, a medical grade cement which is visible on X-ray imaging is injected. The cement mixture resembles thick toothpaste and sets hard within 20 minutes. The interventional radiologist will monitor the entire procedure on the x-ray monitors to ensure the cement fills the fractured vertebrae adequately and does not leak into the spinal canal or adjacent blood vessels. Small cement leaks into the adjacent soft tissues may occur but very rarely cause any problems.
The procedure usually takes about one hour but can take longer if more than one level is being treated.
What do patients experience during/after the procedure?
Patients lie face down throughout the procedure. The medications given prior to and during the procedure help to ensure that patients remain calm and sleepy, also minimising any discomfort. The vertebroplasty procedure is generally very well tolerated.
Bed rest is recommended for the first 3 hours following vertebroplasty, although after 1 hour patients can get up to use the bathroom if they so choose. Most outpatients go home the same day whilst inpatients usually remain in hospital whilst their pain medications are reduced and they have physiotherapy to regain mobility.
Following discharge, patients are advised to gradually increase physical activity and resume all regular medications. Blood thinners are usually restarted on the day of the procedure.
What are the benefits versus the risks?
Benefits
Because the pain of a vertebral fracture is helped by vertebroplasty, patients feel significant relief within hours or days after the procedure. Within days or weeks, two-thirds of patients are able to lower their doses of pain medication significantly.
About 75% of patients regain lost mobility and become more active. This increase in activity helps to combat osteoporosis and improve cardiovascular fitness.
Risks
Vertebroplasty is a relatively safe procedure with a low risk of serious complication.
The most serious potential risk is if a cement leak presses upon the spinal cord or an adjacent nerve. In the worst case, this could require an emergency operation. We consider the risk of this occurring to be less than 1 in 1000. There are reports of cement leaking into an adjacent vein and then being transported through the body to the lungs potentially causing breathing problems. Again, this is very unlikely and we consider the risk also to be less than 1 in 1000.
Discomfort, infection and bleeding are the other risks which are associated with all invasive procedures.
What are the limitations of vertebroplasty?
Vertebroplasty does not treat herniated disks or arthritic back pain and will not correct a curvature of the spine secondary to fractures, but may prevent any curvature from worsening.
It can be difficult for some patients with severe lung and heart disease to lie face down for the procedure. The healthcare team will try to make special accommodations for a patient with these types of conditions.
If you have any further questions please make a note of them and ask the doctor who will perform your procedure.

